Irritable Bowel Syndrome (IBS): Overview
Tara Carpenter, NC.
Holistic nutrition for people on The Body Ecology Diet (B.E.D.).

What is IBS?
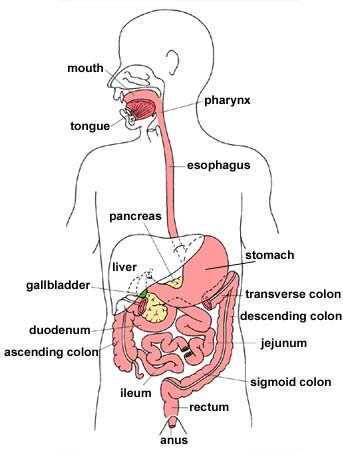
IBS is a collection of symptoms in the gastrointestinal (GI) system yet can be present throughout the body and mind. This condition affects delicate timing of peristalsis movement, digestive secretions, and food absorption; with about 10-20% adults in U.S. are affected, with most diagnosed in their 20’s, 30’s, and 40’s.
Too Fast, Too Slow
IBS symptoms come mainly from the large intestinal muscle contracting either too rapidly or too slowly when compared to normal. Also, from the autonomic nervous and digestive system functioning less than harmonious to produce effortlessly and painless bowel movements.
When intestinal contractions (peristalsis) move too rapidly, then the food you eat moves too quickly through the GI tract and the result is that the intestinal wall will not have enough time to absorb/extract the liquids and nutrients from food particles passing by. This tends to result in a state of malnourishment and diarrhea. Contractions that are too slow give the intestinal walls too much time to absorb liquids from the stool and result in constipation or pellet-like bowel movement.
3 Types of IBS
- Diarrhea-dominant: discomfort, bowel urgency, frequency, loose stool.
- Constipation-dominant: discomfort, delayed, infrequent, hard stool.
- Alternating bouts of diarrhea and constipation.
The Rome III Diagnostic Criteria for Functional GI Disorders says IBS is abdominal discomfort (uncomfortable sensation, not pain) lasting 3 days, has occurred in last 3 months, and associated with 2+ of following:
- Improvement with defecation.
- Onset associated with change in stool frequency.
- Onet associated with change in stool appearance.

Signs & Symptoms
- Crampy abdominal feelings
- No structural abnormalities
- Anorexia
- Anxiety, depression, stress
- Back or urinary pain
- Constipation
- Diarrhea, often in morning
- Bloated
- Gas (flatulence)
- Grumbling gut
- Incomplete evacuation
- Increased pain sensitivity
- Mucus in stool
- Pellets or pencil-thin stool
- Stomach numbing
- Sensitivity in lower left abdomen, relief from pooping
Risk Factors
Anyone can be diagnosed, including kids and elders, yet more likely women, young adults, and anyone with IBS family history, or depression/anxiety.
Diagnosis
There is no single test to confirm IBS. Instead, doctors look at symptoms and family history and rule out other conditions like IBS with a blood test for inflammatory bowel disease (includes Crohn’s disease, ulcerative colitis, Celiac disease, anemia). They may also do a hydrogen breath test to check for lactose intolerance, colonoscopy for rectal bleeding and colon cancer, or take a stool sample to check for malabsorption if diarrhea is present.

Causes & Triggers
- Stress, whether from food sensitivities (#1 stress for many), emotions, pain, toxins, infection, or prolonged stress can lead to intestinal permeability and less good gut flora. Stress alters bacteria and evidence supports role of altered small intestine microbiota/dysbiosis.
- Miscommunication between brain and gut, related to serotonin neurotransmitter; responsible for motility/pain sensation in GI tract.
- Genetic studies show IBS runs in families; no specific gene found.
- Infection is a factor in IBS and can lead to a disruption in gut flora and damaged intestinal wall nerves.
- Inflammation inside of gut presents as high levels of specific cytokines, making it a piece of the IBS puzzle.
- Research indicates IBS may be due to gut dysbiosis/Small Intestinal Bacteria Overgrowth (SIBO).
This handout may contain affiliate links, please read here to learn more.
Disclaimer: This is general information only; primarily educational in nature; and is not a substitute for the medical advice of your health care professional that you require for any cause whatsoever, now or in future. Please consult a medical doctor before implementing diet and lifestyle changes mentioned and continue any existing treatments unless your doctor says otherwise.
May all bellies be happy!
References
Bauman, E., Friedlander, J. (2011). Therapeutic Nutrition. Penngrove, CA: Bauman.
Nichols, T., Favas, N. (2005). Optimal Digestive Health. Rochester, VT: Healing Arts Press.
Pimentel, Mike. A New IBS Solution. (2006).
Catsos, Patsy. IBS-Free at Last. Portland, ME: Pond Cove Press, 2008.
Magee, Elaine. Tell Me What to Eat for IBS .